Many people experience the discomfort of acid reflux – that burning sensation in your chest, the sour taste in your mouth, sometimes even difficulty swallowing. It’s a common ailment, and often seems to flare up after eating, particularly late at night. This leads many to wonder: is there a direct link between when you eat and experiencing these unpleasant symptoms? The intuitive feeling that late-night snacking or dinner is somehow responsible isn’t unfounded, but the relationship is more complex than simply blaming the clock. Understanding the physiological processes involved, how our bodies change as night falls, and individual factors all play crucial roles in determining whether a late meal will trigger acid reflux.
The human digestive system doesn’t operate on a strict schedule; it’s constantly working, even while we sleep. However, its activity levels do fluctuate throughout the day, influenced by hormones, food intake, and body position. When we eat, the stomach produces hydrochloric acid to break down food. Normally, this process is well-regulated, and mechanisms are in place to prevent stomach acid from flowing back up into the esophagus – the muscular tube connecting your mouth to your stomach. But these protective mechanisms can be compromised, leading to reflux. The timing of meals, combined with other lifestyle factors, can significantly impact how effectively these systems function and ultimately determine whether you experience heartburn or related symptoms. This article will explore the nuances of this relationship, debunking myths and providing a deeper understanding of why late-night eating sometimes triggers acid reflux. You might also wonder are you eating too late and how it impacts digestion.
Understanding Acid Reflux and its Causes
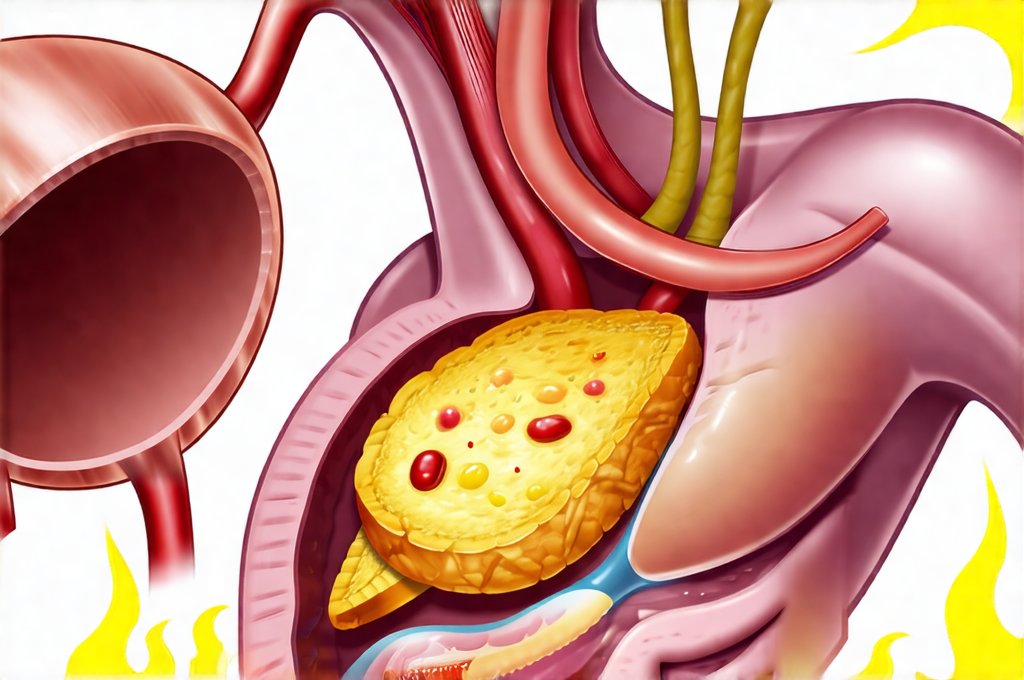
Acid reflux occurs when stomach acid flows back up into the esophagus. This is often referred to as heartburn, although it’s important to remember that heartburn is simply a symptom, not the underlying cause. Several factors can contribute to this backward flow of stomach contents, making some individuals more prone to experiencing reflux than others. These include:
- A weakened lower esophageal sphincter (LES): This muscular valve at the bottom of the esophagus should remain tightly closed except when swallowing.
- Hiatal hernia: A condition where part of the stomach pushes up through the diaphragm, weakening the LES.
- Obesity: Excess weight can increase pressure on the abdomen and force acid upwards.
- Certain foods: Fatty foods, spicy foods, chocolate, caffeine, alcohol, and acidic foods (like citrus fruits and tomatoes) are known triggers for some people.
- Pregnancy: Hormonal changes and increased abdominal pressure during pregnancy can contribute to reflux.
- Smoking: Weakens the LES and increases stomach acid production.
While these factors represent common causes, they don’t fully explain why late-night eating is often associated with worsened symptoms. It’s not necessarily what you eat, but when you eat in relation to your body’s natural rhythms that can exacerbate reflux. Our digestive system naturally slows down as we prepare for sleep, and lying flat shortly after a meal increases the likelihood of acid flowing back up into the esophagus. This is because gravity normally helps keep stomach contents down. It’s helpful to start with what is acid reflux to understand the basics.
The connection isn’t always straightforward; some individuals can eat late without experiencing any issues, while others are highly sensitive even to small nighttime snacks. Individual variations in LES strength, overall digestive health, and sensitivity to acid all play a role. It’s crucial to understand that there is no one-size-fits-all answer. Can eating too quickly contribute to these symptoms?
The Role of Body Position and Digestion
As mentioned previously, gravity plays a significant role in preventing acid reflux. When we stand or sit upright, gravity helps keep stomach contents where they belong. However, when we lie down, particularly shortly after eating, gravity works against us, making it easier for stomach acid to travel back up the esophagus. This is why many people experience worse heartburn at night.
Digestion also slows down considerably as we prepare for sleep. The body prioritizes rest and repair over active digestion during nighttime hours. This slower digestive process means food stays in the stomach longer, increasing the risk of acid production and potential reflux. Furthermore, hormonal changes occur overnight that can impact digestive function. For example, levels of gastrin, a hormone that stimulates acid production, tend to rise at night. This combination of factors—body position, slowed digestion, and hormonal shifts—creates an environment where late-night eating is more likely to trigger reflux symptoms.
It’s also important to consider the type of food consumed before lying down. High-fat foods take longer to digest, increasing the amount of time stomach acid is produced. Large meals can overwhelm the digestive system, making it harder for the LES to stay closed. Therefore, even if you don’t normally experience reflux, a large, fatty meal close to bedtime could potentially trigger symptoms. Are you eating too many trigger foods at once?
Identifying Your Personal Triggers
The key to managing acid reflux effectively is understanding your individual triggers. What sets off one person’s heartburn may not affect another. Here are some steps you can take to identify your personal triggers:
- Keep a food diary: Record everything you eat and drink, along with the time of day and any associated symptoms. This will help you pinpoint specific foods or meals that seem to worsen your reflux.
- Pay attention to timing: Note when you ate your last meal before bed and whether it coincided with heartburn symptoms. Experiment with adjusting your eating schedule.
- Observe body position: Do you experience more reflux when lying flat versus propped up? This can help determine if gravity is a significant factor for you.
- Consider other factors: Stress, smoking, and certain medications can also contribute to acid reflux. Take these into account when evaluating your symptoms.
Once you’ve identified potential triggers, you can begin making adjustments to your diet and lifestyle to minimize symptoms. This might involve avoiding specific foods, eating smaller meals, or elevating the head of your bed. Perhaps can intuition guide these decisions?
Lifestyle Adjustments for Reflux Management
Beyond identifying your personal triggers, several lifestyle modifications can help reduce acid reflux:
- Elevate the head of your bed by 6-8 inches: This uses gravity to your advantage and helps prevent stomach acid from flowing upwards while you sleep. You can achieve this with bed risers or a wedge pillow.
- Avoid eating large meals before bedtime: Aim for smaller, more frequent meals throughout the day.
- Limit fatty foods, spicy foods, chocolate, caffeine, alcohol, and acidic foods: These are common triggers for many people.
- Maintain a healthy weight: Obesity increases abdominal pressure, contributing to reflux.
- Quit smoking: Smoking weakens the LES and increases stomach acid production.
- Manage stress: Stress can exacerbate digestive issues. Practice relaxation techniques like yoga or meditation.
These adjustments can often significantly reduce the frequency and severity of acid reflux symptoms without requiring medication. However, if lifestyle changes are insufficient, it’s important to consult with a healthcare professional.
When to Seek Medical Attention
While occasional heartburn is usually not cause for concern, certain symptoms warrant medical attention:
- Frequent or severe heartburn that doesn’t respond to over-the-counter medications.
- Difficulty swallowing (dysphagia).
- Persistent nausea or vomiting.
- Chest pain, especially if accompanied by shortness of breath or jaw/arm pain – this could be a sign of a heart attack.
- Unintentional weight loss.
These symptoms may indicate a more serious underlying condition, such as gastroesophageal reflux disease (GERD) or esophagitis. A healthcare professional can diagnose the cause of your symptoms and recommend appropriate treatment options, which might include medications like proton pump inhibitors (PPIs) or H2 blockers. Self-treating chronic acid reflux without medical guidance is not recommended. Can acid reflux cause ear pain?
In conclusion, while late-night eating can contribute to acid reflux for many people, it’s rarely the sole culprit. The relationship is complex and influenced by a multitude of factors, including individual physiology, body position, dietary choices, and lifestyle habits. By understanding these nuances and taking steps to identify your personal triggers, you can effectively manage your symptoms and improve your overall digestive health. Remember that proactive management and seeking professional advice when necessary are key to living comfortably with acid reflux. Can eating the same food every day cause reactions?