The chest pain is gripping, tight, radiating down the left arm… instantly triggering panic. For many, this immediately conjures images of a heart attack – a potentially life-threatening event demanding immediate emergency care. But what if that intense discomfort isn’t cardiac in origin? What if it’s stemming from something entirely different, yet capable of mimicking the most frightening symptom of a heart attack with startling accuracy? This is where gastroesophageal reflux disease (GERD) enters the picture, often underestimated as merely “heartburn,” but possessing the power to create symptoms so similar to cardiac emergencies that differentiating between the two can be incredibly challenging – and crucial.
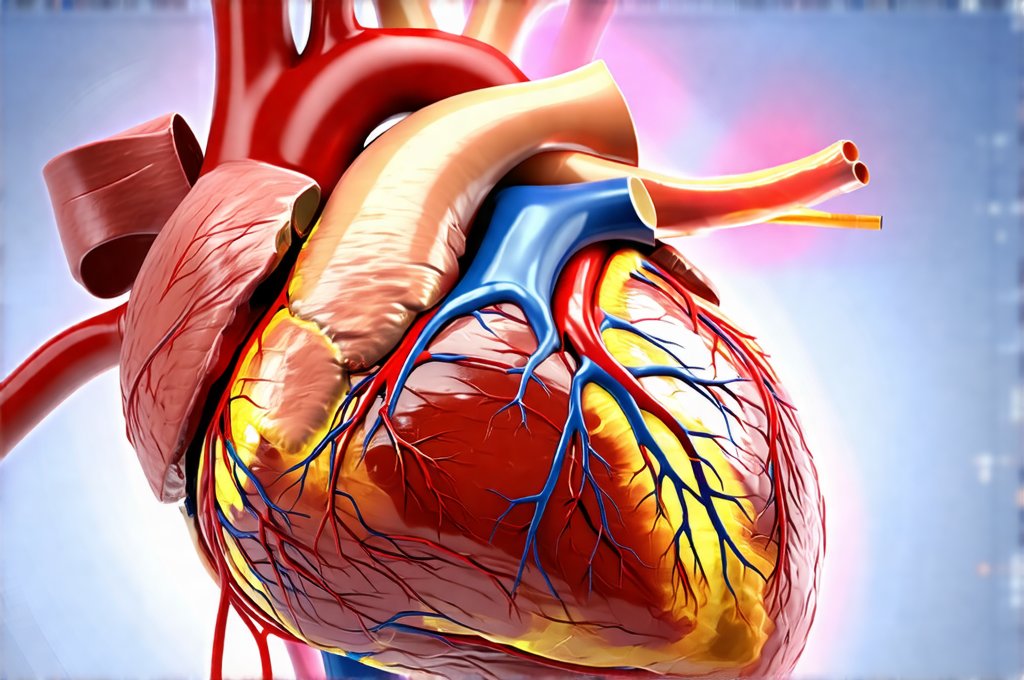
The overlap in symptoms between GERD and a heart attack isn’t coincidence; it’s rooted in shared nerve pathways and proximity of organs. Both conditions can cause chest pain, shortness of breath, and even radiating discomfort. The esophagus, where reflux occurs, sits relatively close to the heart, and both are innervated by similar nerves. This means that signals from esophageal irritation or spasms can be misinterpreted by the brain as originating from the heart itself. While recognizing these similarities is important for awareness, it’s never a justification for self-diagnosis; prompt medical evaluation remains paramount when experiencing chest pain.
Understanding GERD and Its Manifestations
Gastroesophageal reflux disease (GERD) occurs when stomach acid frequently flows back into the esophagus – the muscular tube connecting your mouth to your stomach. This backflow, called acid reflux, irritates the lining of the esophagus, causing that familiar burning sensation we typically associate with heartburn. However, GERD is much more than just occasional heartburn. It’s a chronic condition with a wide spectrum of symptoms, varying significantly from person to person. Some individuals experience classic heartburn and regurgitation (the sensation of stomach contents coming back up), while others present with atypical symptoms that can easily be mistaken for other illnesses – including heart problems.
These atypical GERD symptoms are what make diagnosis tricky. Beyond the typical burning in your chest, you might experience: chronic cough, hoarseness, difficulty swallowing (dysphagia), sore throat, and even asthma-like wheezing. Crucially, these can all accompany or masquerade as cardiac pain. The intensity of GERD symptoms isn’t necessarily tied to the severity of esophageal damage; someone with mild inflammation can experience intense pain, while another with significant damage might have minimal discomfort. This variability adds to the complexity of distinguishing GERD from heart conditions. If you struggle with identifying what you can eat, consider comfort foods that won’t exacerbate your symptoms.
The underlying causes of GERD are multifaceted. A weakened lower esophageal sphincter (LES) – a muscular valve that should prevent acid reflux – is often a key factor. Hiatal hernias, where part of the stomach protrudes through the diaphragm, can also contribute. Lifestyle factors such as obesity, smoking, diet choices (fatty or spicy foods, caffeine, alcohol), and certain medications can exacerbate symptoms. Understanding these contributing factors allows for targeted lifestyle modifications to help manage the condition. Many find it helpful to cook specifically for a sensitive stomach as well.
Dissecting the Overlap: GERD vs. Heart Attack Symptoms
The core issue lies in the shared symptom of chest pain. A heart attack typically presents with a crushing, squeezing, or heavy pressure in the chest, often radiating to the left arm, jaw, neck, or back. It’s frequently accompanied by shortness of breath, nausea, sweating, and a feeling of impending doom. However, GERD-related chest pain can mimic these sensations remarkably well. The key differences are subtle but critically important. GERD pain is more likely to be described as burning or acidic, and it often worsens after eating or when lying down. It may also be relieved by antacids.
However, relying on these distinctions alone isn’t enough. Many heart attacks present atypically, particularly in women, the elderly, and individuals with diabetes. Atypical heart attack symptoms can include mild chest discomfort, fatigue, shortness of breath without chest pain, or even abdominal pain. This overlap is why it’s so dangerous to self-diagnose. If you’re experiencing chest pain, especially if it’s new, severe, or accompanied by other concerning symptoms like sweating, dizziness, or profound weakness – call emergency services immediately. It’s always better to err on the side of caution. To help manage daily life with GERD, building a morning routine can be extremely beneficial.
Recognizing Atypical Presentations and Risk Factors
Atypical presentations are the biggest challenge in differentiating between GERD and a heart attack. Individuals with pre-existing conditions like anxiety can also experience chest pain that mimics cardiac events, further complicating matters. Furthermore, some people simply don’t feel chest pain during a heart attack; they might only feel extreme fatigue or shortness of breath. This is why understanding your personal risk factors for both GERD and heart disease is vital. Risk factors for heart disease include: high blood pressure, high cholesterol, diabetes, smoking, family history of heart disease, obesity, and lack of physical activity.
For GERD, risk factors encompass those listed earlier – hiatal hernia, obesity, smoking, dietary choices, certain medications (like NSAIDs), and pregnancy. It’s important to note that these aren’t mutually exclusive; someone can have both risk factors for heart disease and GERD, increasing their vulnerability to experiencing overlapping symptoms. If you fall into any high-risk category, regular checkups with your doctor are essential. You may also want to consider how to test for sensitivities without a lab to help narrow down triggers.
When to Seek Immediate Medical Attention – and What to Expect
If you’re experiencing chest pain, treat it as a potential emergency until proven otherwise. Don’t hesitate to call emergency services (911 in the US) or go to the nearest emergency room. Explain your symptoms clearly and accurately to the medical professionals. They will likely perform tests to determine the cause of your chest pain. These may include: an electrocardiogram (ECG/EKG) to assess heart rhythm, blood tests to check for cardiac enzymes (markers of heart damage), and potentially a chest X-ray.
If GERD is suspected, further testing might involve an endoscopy – where a thin, flexible tube with a camera is inserted into the esophagus to visualize the lining – or esophageal manometry – which measures the pressure within the esophagus. Importantly, even if initial tests suggest GERD, doctors may still monitor you for signs of cardiac involvement, especially if symptoms are severe or atypical. Remember that accurate diagnosis is paramount and requires professional medical evaluation. Self-treating based on assumptions can have serious consequences. Planning ahead with a travel kit for gut health can also help to manage symptoms while away from home, and learning how to eat on a budget can make managing GERD more accessible. Finally, a rotation diet may help you identify trigger foods.