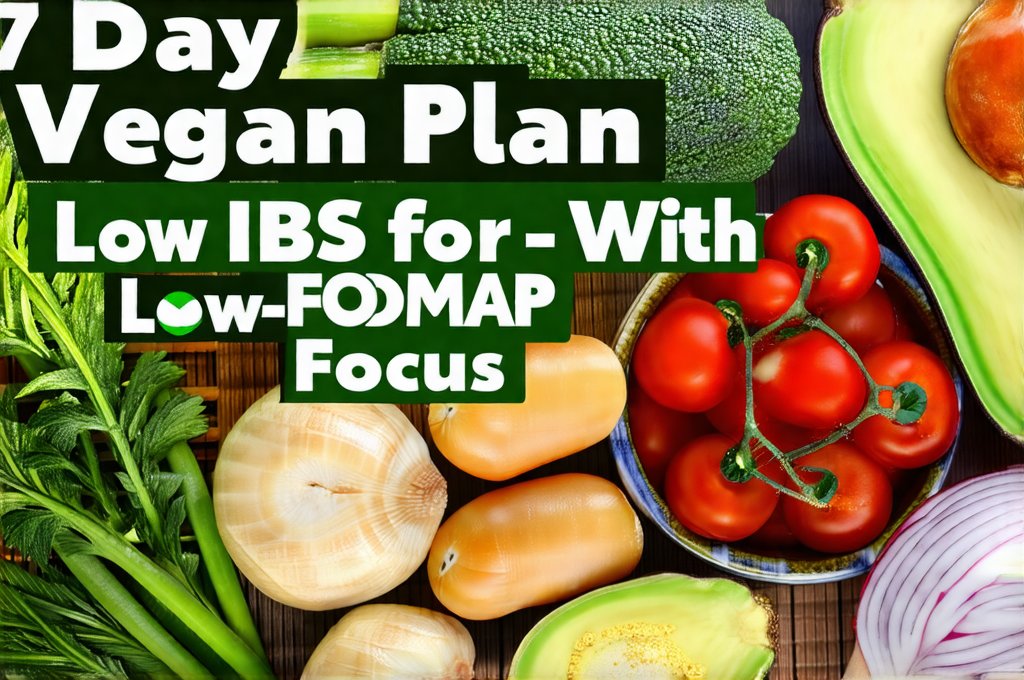
Living with Irritable Bowel Syndrome (IBS) can be incredibly challenging, often requiring significant dietary adjustments to manage symptoms. For those embracing a vegan lifestyle, navigating IBS restrictions can feel even more complex. Many plant-based staples – beans, lentils, certain fruits and vegetables – are high in FODMAPs (Fermentable Oligosaccharides, Disaccharides, Monosaccharides, And Polyols), substances that can trigger digestive distress in susceptible individuals. However, a vegan diet can be IBS-friendly; it simply requires careful planning and understanding of low-FODMAP principles. This 7-day plan aims to provide a starting point for incorporating delicious, nourishing, and gut-friendly vegan meals into your routine while minimizing potential IBS triggers. It’s designed as a guide, recognizing that individual tolerances vary considerably, so listening to your body is paramount.
This isn’t about restriction for the sake of it; it’s about empowerment through knowledge. Understanding how different foods impact your digestive system is key to long-term success. This plan focuses on readily available ingredients and relatively simple recipes, making it sustainable even with a busy lifestyle. It’s also important to remember that this is not intended as a substitute for professional medical advice. If you have been diagnosed with IBS, or suspect you might, please consult a registered dietitian or healthcare provider specializing in gut health to personalize your dietary approach based on your specific needs and sensitivities. We will be focusing on the elimination phase of a low-FODMAP diet, aiming to identify trigger foods and then gradually reintroduce them as tolerated. Nutrition Support For Individuals With Digestive Motility Disorders Or IBS can provide further guidance on this topic.
Understanding Low-FODMAP Veganism
The core principle of this plan is minimizing FODMAP intake. This means being mindful of ingredients often found in vegan diets that can exacerbate IBS symptoms. High-FODMAP vegan foods include: onions, garlic, apples, pears, stone fruits (peaches, plums), honey, high fructose corn syrup, wheat and rye products, beans, lentils, chickpeas, and certain vegetables like broccoli and cauliflower in large quantities. Luckily, there are plenty of delicious low-FODMAP alternatives available! Rice, oats, quinoa, potatoes, carrots, spinach, bananas, blueberries, oranges, and lactose-free plant milks (almond, rice, coconut) form the foundation of many recipes within this plan. Monash University’s FODMAP Diet app is an invaluable resource for checking the FODMAP content of individual foods.
Navigating a low-FODMAP vegan diet requires some label reading and ingredient awareness. Many processed vegan products contain high-FODMAP ingredients, so opting for whole, unprocessed foods whenever possible is generally best. For example, choose gluten-free tamari instead of regular soy sauce, and look for plant-based yogurts made without inulin or chicory root fiber (common FODMAPs). Don’t be afraid to experiment with spices and herbs to add flavor – many are naturally low-FODMAP! Focusing on the abundance of what can you eat, rather than dwelling on restrictions, will make this dietary journey more enjoyable and sustainable. Choosing The Right Cooking Oils For People With Reflux, Nausea, Or IBS can help you select appropriate fats for cooking and flavoring your meals.
It’s also important to consider portion sizes. Even low-FODMAP foods can cause symptoms if consumed in excessive amounts. For instance, while a small serving of spinach is generally well-tolerated, a large salad might trigger discomfort. This plan provides guidance on appropriate serving sizes, but again, individual tolerance levels vary considerably.
7-Day Vegan Meal Plan (Low-FODMAP Focus)
This meal plan offers a sample structure for each day. Feel free to swap meals between days based on your preferences and what you have available. Remember to drink plenty of water throughout the day – staying hydrated is crucial for digestive health. Portion sizes are approximate and can be adjusted based on individual needs. Snacks are included, but feel free to add or adjust them as required.
Day 1: Breakfast: Oatmeal (made with lactose-free rice milk) topped with blueberries and a sprinkle of chia seeds. Lunch: Quinoa salad with shredded carrots, spinach, cucumber, and a lemon-tahini dressing. Dinner: Baked potato with roasted bell peppers and a side of steamed green beans. Snack: Small banana.
Day 2: Breakfast: Smoothie made with lactose-free almond milk, banana, spinach, and a tablespoon of peanut butter. Lunch: Rice noodles with stir-fried tofu and low-FODMAP vegetables (carrots, zucchini). Dinner: Vegan “chicken” (made from textured vegetable protein) and roasted potatoes with rosemary. Snack: Orange slices.
Day 3: Breakfast: Gluten-free toast with avocado and a sprinkle of hemp seeds. Lunch: Leftover vegan “chicken” and potatoes. Dinner: Red lentil & rice soup (using red lentils – these are lower in FODMAPs than other varieties). Snack: Rice cakes with peanut butter. Low-Fiber Diet for IBS with Diarrhea can help you understand fiber intake and manage symptoms.
Day 4: Breakfast: Chia seed pudding made with lactose-free coconut milk and topped with strawberries. Lunch: Large salad with mixed greens, cucumber, carrots, and a vinaigrette dressing. Dinner: Vegan Shepherd’s pie (using mashed potatoes as the topping and low-FODMAP vegetables). Snack: Small handful of blueberries.
Day 5: Breakfast: Oatmeal with sliced banana and walnuts. Lunch: Leftover vegan shepherd’s pie. Dinner: Stir-fried tofu with rice noodles and a ginger-soy sauce (gluten-free tamari). Snack: Rice crackers. Easy 7-Day Acid Reflux Meal Plan With Snacks offers additional meal ideas that may be compatible with your needs.
Day 6: Breakfast: Smoothie made with lactose-free almond milk, pineapple, and spinach. Lunch: Quinoa salad with cucumber, carrots, and bell peppers. Dinner: Baked sweet potato with black beans (small portion) & avocado. Snack: Small apple slices.
Day 7: Breakfast: Gluten-free toast with peanut butter and sliced banana. Lunch: Leftover baked sweet potato with black beans and avocado. Dinner: Vegetable curry made with coconut milk, potatoes, carrots, and spinach (avoiding onion/garlic). Snack: Orange.
Navigating Common Challenges
One of the biggest hurdles in low-FODMAP veganism is finding suitable alternatives to traditional flavor enhancers like garlic and onions. Fortunately, there are several ways to achieve delicious flavor without these ingredients. Asafoetida (hing) is a spice commonly used in Indian cuisine that can mimic the savory depth of garlic and onion when used sparingly. Infusing oils with ginger or chili peppers can also add complexity to dishes. Furthermore, herbs like rosemary, thyme, oregano, and basil are excellent low-FODMAP flavor boosters.
Another challenge arises from the potential for hidden FODMAPs in processed foods. Always read ingredient lists carefully and be wary of ingredients like inulin, chicory root fiber, high fructose corn syrup, and honey. Choosing whole, unprocessed foods as much as possible minimizes this risk. Preparing your own meals also gives you complete control over what goes into your food, ensuring that it aligns with your dietary needs.
Finally, remember to listen to your body. Even with careful planning, individual tolerances vary considerably. If a particular food triggers symptoms, eliminate it from your diet and reintroduce it later in small amounts to assess your tolerance level. Keeping a food diary can be immensely helpful in identifying trigger foods and understanding your unique sensitivities. Travel Tips for Individuals with IBS can help you manage symptoms when on the go.
Reintroduction Phase & Long-Term Management
After the initial elimination phase (typically 2-6 weeks), carefully reintroducing FODMAPs one by one is crucial. This allows you to identify which specific FODMAPs are causing symptoms and at what quantities. Start with small portions of a single FODMAP group, such as fructose or lactose, and monitor your symptoms for several days before introducing another. If you experience significant discomfort, discontinue the reintroduction and wait until symptoms subside before trying again.
Long-term management involves finding a balance between restriction and enjoyment. The goal isn’t necessarily to eliminate all FODMAPs forever, but rather to identify your individual trigger foods and adjust your diet accordingly. Many people with IBS can tolerate small amounts of certain FODMAPs without experiencing significant symptoms. Fermented Alternatives To Yogurt For Those With Dairy Sensitivity offers options to support gut health. Working with a registered dietitian specializing in gut health is highly recommended during this phase to develop a personalized long-term dietary plan. The Link Between Gut Microbiota And IBS With Diarrhea Vs Constipation highlights the importance of gut health in managing IBS symptoms.
Ultimately, successful vegan IBS management requires ongoing self-awareness, mindful eating, and a commitment to understanding your body’s unique needs. It’s about finding a sustainable approach that allows you to enjoy delicious, nutritious food without compromising your digestive health. Remember that this is a journey, not a destination, and there will be ups and downs along the way. Be patient with yourself, celebrate small victories, and prioritize your well-being.