Indigestion, something many experience occasionally after a large meal or spicy food, becomes concerning when it’s chronic – a persistent companion rather than a fleeting discomfort. Long-term indigestion isn’t merely an annoyance; it signals potential problems within the digestive system, often involving repeated exposure of the esophagus to stomach acid. This consistent irritation can trigger a cascade of changes, not only affecting the physical structure of the esophagus itself but also profoundly altering eating habits and overall quality of life. Understanding this interplay between prolonged indigestion, esophageal damage, and behavioral shifts is crucial for recognizing when professional help is needed and proactively managing digestive health.
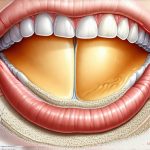
The esophagus, that muscular tube connecting your throat to your stomach, isn’t designed to withstand frequent acid baths. While occasional reflux is normal, the constant backflow of acidic stomach contents – often associated with long-term indigestion – can lead to significant structural changes. This prolonged exposure doesn’t just cause heartburn; it sets the stage for more serious conditions that require medical attention and can dramatically impact how we relate to food, from what we choose to eat to how comfortably we can consume it. It’s a cycle where physical damage influences dietary choices, which can then exacerbate the initial problem, creating a challenging and often frustrating situation.
Esophageal Damage: From Reflux to Serious Conditions
The primary way long-term indigestion leads to esophageal damage is through gastroesophageal reflux disease (GERD). GERD isn’t simply “bad heartburn”; it’s a chronic condition where stomach acid frequently flows back into the esophagus. This happens when the lower esophageal sphincter (LES) – a muscular valve at the bottom of the esophagus – weakens or relaxes inappropriately. When this occurs, acidic contents irritate the delicate lining of the esophagus, leading to inflammation and potential structural changes over time. – The severity of GERD can range from mild, manageable symptoms to severe complications requiring intervention. Understanding how acid response plays a role is also important.
Beyond simple irritation, persistent acid exposure can lead to several specific esophageal conditions. Esophagitis – inflammation of the esophagus – is a common first step. If left unchecked, chronic esophagitis can progress to more serious issues like esophageal strictures (narrowing of the esophagus) which make swallowing difficult, and Barrett’s esophagus, a precancerous condition where the normal lining of the esophagus changes. Barrett’s esophagus increases the risk of developing esophageal adenocarcinoma, a relatively rare but aggressive form of cancer. This progression underscores the importance of addressing chronic indigestion promptly and effectively.
The development of these conditions isn’t always linear or obvious. Many people experience years of seemingly mild symptoms, masking the underlying damage occurring within the esophagus. It’s this slow, insidious nature that makes early detection so critical. Lifestyle modifications and medical interventions can often halt or even reverse some of these changes, but delaying treatment allows the damage to accumulate, potentially leading to more significant health problems down the line.
Altered Eating Habits: A Vicious Cycle
Chronic indigestion and the resulting esophageal damage frequently lead to dramatic alterations in eating habits. Initially, individuals might start avoiding foods that trigger heartburn – spicy dishes, fatty foods, citrus fruits, caffeine, alcohol – creating a self-imposed dietary restriction. While this may provide temporary relief, it can also lead to nutritional deficiencies and an overall diminished enjoyment of food. – These restrictions are often driven by fear of triggering symptoms rather than actual allergies or intolerances.
As esophageal damage progresses, the act of swallowing itself can become painful or difficult. This leads to further modifications in eating behavior, such as: 1. Eating smaller, more frequent meals. 2. Avoiding solid foods altogether and opting for liquids or purees. 3. Eating very slowly and deliberately. These changes aren’t simply preferences; they are coping mechanisms developed to minimize discomfort. However, these alterations can inadvertently exacerbate the problem by reducing esophageal motility (the ability of the esophagus to move food down) and contributing to further acid reflux.
The psychological impact shouldn’t be underestimated either. Constant worry about triggering symptoms can lead to food anxiety – a state of heightened stress surrounding mealtimes. This anxiety can result in social isolation, as individuals may avoid eating out or sharing meals with others for fear of experiencing discomfort. Over time, this creates a vicious cycle where physical damage and psychological distress reinforce each other, significantly impacting quality of life and overall well-being. It’s important to remember that seeking help isn’t just about addressing the physical symptoms; it’s also about reclaiming control over your relationship with food and restoring enjoyment in everyday activities. Understanding how energy levels can be impacted by GERD is important too.
Diagnostic Tools & Seeking Help
Diagnosing the extent of esophageal damage typically involves several tests. Endoscopy, where a thin, flexible tube with a camera is inserted into the esophagus, allows doctors to directly visualize the lining and identify any inflammation, ulcers, or Barrett’s esophagus. Biopsies can be taken during endoscopy to check for precancerous changes. – Other diagnostic tools include esophageal manometry, which measures the pressure within the esophagus and LES function, and pH monitoring, which assesses the amount of acid reflux over a 24-hour period.
It’s vital to seek medical attention if you experience persistent indigestion, heartburn that doesn’t respond to over-the-counter medications, difficulty swallowing (dysphagia), or unexplained weight loss. A healthcare professional can accurately diagnose the underlying cause and recommend an appropriate treatment plan. Treatment options may include: 1. Lifestyle modifications (dietary changes, elevating the head of your bed). 2. Medications (antacids, H2 blockers, proton pump inhibitors). 3. In more severe cases, surgery to strengthen the LES or manage complications. Long-term antacid use should be discussed with your doctor.
Remember: self-treating chronic indigestion can mask underlying problems and delay necessary medical intervention. Early diagnosis and consistent management are key to preventing serious complications and maintaining long-term digestive health. Don’t hesitate to discuss your concerns with a doctor – proactive care is essential for protecting your esophagus and enjoying a comfortable, fulfilling life. Additionally, consider how concentration can be affected by GERD. Finally, understanding how weather impacts acid reflux symptoms is helpful for managing your condition.